
One of the most common diseases today isosteochondrosis of the lumbar spine. Both men and women turn to doctors with this disease equally often.
Each of us has experienced pain in the lower back, sacrum or lower extremities at least once in our life. We often unconsciously refer to this type of pain as "pinched nerve in the lower back".
Causes of lumbar osteochondrosis
According to research by doctors and scientists, the main cause of osteochondrosis of the lumbar spine is upright posture. However, not all people suffer from osteochondrosis. The provoking factors that accelerate the development of the disease are: metabolic disorders, physical inactivity, injuries, excess weight, improper weight lifting.
The source of pain in osteochondrosis is the pinching of nerve roots, which occurs after the protrusion of the intervertebral disc and the narrowing of the intervertebral gap. This deviation occurs when nutrition deteriorates, the natural processes of oxygen and lymph exchange in the tissues of the intervertebral discs are disrupted. As a result, the capacity of the intervertebral discs decreases, and the nucleus pulposus of the disc gradually shrinks and dries up.
From an anatomical point of view, lumbar osteochondrosis is a process of transformation of cartilage into bone, which results in excessive pressure on the roots of nerves extending from the spinal cord. This change causes pain. Excessive growth of bone tissue occurs due to deterioration of nutrition of intervertebral discs, loss of fluid and disturbances in structure and functioning.
When the protrusion of the intervertebral disc during the development of osteochondrosis of the lumbar spine becomes more serious, it causes the development of lumbar protrusion and herniation of the lumbar disc due to the rupture of the fibrous ring.
The pain syndrome occurs due to pinching of the spinal nerve in lumbar osteochondrosis and is called lumboischialgia. This symptom is accompanied by numbness of the lower extremities. Depending on the nature and localization of the pain, the disease can be divided into sciatica and lumbago. Inflammation of a nerve due to its pinching is called radiculitis. The methods of treating radiculitis with painkillers are, in fact, only the removal of symptoms, and they are ineffective, because such treatment does not affect the real cause of the disease, which is the degenerative processes in the intervertebral discs. In order to eliminate pain and take preventive measures to prevent complications, it is necessary to undergo a comprehensive treatment to activate the restoration processes in the disc tissues, normalize the height and physiological parameters of the intervertebral discs.
Symptoms of osteochondrosis of the lumbar spine

One of the signs of osteochondrosis is the compression of spinal nerve roots by the protruding nucleus pulposus of the intervertebral disc. This compression occurs in the epidural space, which is a sort of container for the spinal roots. Osteochondrosis of the lumbar spine is manifested by the following symptoms corresponding to the compressed root:
- L1 and L2 – loss of sensitivity in the "rider's pants" area, i. e. in the groin area and inner thighs. Pain can appear in both legs at once if lumbar osteochondrosis is complicated by the development of a hernia.
- L5 – shooting pain, decreased sensitivity in the lower back and thumb, and decreased ability to flex the finger.
- S1 – shooting pain, reduced sensitivity of the lower leg and outer side of the upper leg, pain in the foot from the little to the fourth toe. Often when this root is damaged, the Achilles and plantar reflexes are lost.
- Damage to the Deproge-Gotteron artery - in the chronic course of osteochondrosis, paralysis of the lower legs and buttocks may occur, and sensitivity may disappear in the anogenital area.
- Simultaneous damage to L5, S root and Deproge-Gotteron artery causes "paralyzing sciatica" syndrome, loss of pelvic and motor functions.
Osteochondrosis of the lumbar spine can cause protrusions and hernias due to significant loads on this part of the spine. These complications develop very quickly, so it is very important to treat them in time. Do not delay a visit to a vertebrologist, undergo a complete examination and seek qualified help at the first symptoms of lumbar osteochondrosis.
Complications of osteochondrosis of the lumbar spine
Compression-vascular ischemia can be considered a complication of lumbar osteochondrosis. This pathology develops due to disturbed blood supply to the spinal cord, reduction of intervertebral openings for vessels and arteries, as well as narrowing of the peripheral structures of the vertebrae. The reason for the development of this pathology is the flattening of the discs, excessive mobility of the spine, weakened ligaments, the formation of osteophytes and neoatrosis. Permanent injury and pressure on the pinched vessel or artery occurs from any movement of the spinal column that affects the damaged area. In addition, a reflex narrowing of the vessel passing through the constricted canal opening may develop. This effect is called "narrow bed".
Vertebrologists identify another serious complication of osteochondrosis of the lumbar spine. Compressive myelopathy is a disorder of the spinal cord caused by narrowing of the spinal canal. Depending on the location, the symptoms and severity of the pathology may vary. Most often, the course of the disease is episodic - after the attack comes a period of remission.
Lumbar osteochondrosis can be complicated by disc herniation TXII-L1, which exerts pressure and provokes damage to the S1-S2, L2-L-4 segments of the spinal cord. A patient with this complication feels pain in the lower back, lower leg, back of the thigh, as well as weakness in the legs. The gluteal and calf muscles gradually become hypotonic and hypotrophic, the Achilles and plantar reflexes disappear, and foot paresis is formed. The back and outer surfaces of the feet and lower legs are characterized by reduced sensitivity or its complete absence.
If a LI-II disc herniation develops, in which excessive pressure on the caudal segment S3 increases, osteochondrosis of the lumbar spine has the following symptoms: disorder of the pelvic organs, fecal and urinary incontinence, constipation, loss or reduction of sensitivity in the anogenital area, development of decubitus, reflexanal prolapse.
"Cauda equina syndrome" develops when the nerve roots are compressed from the first lumbar vertebra and below. An experienced vertebrologist notes that this syndrome most often develops in patients with congenital narrowing of the spinal canal. "Equina cauda" is a bundle of nerve roots that contains the terminal roots of the spinal cord from the first segment onwards. The name comes from its resemblance to a horse's tail. The diagnosis of this syndrome largely depends on the presence of excruciating pain of a radicular nature. It is this characteristic that distinguishes cauda equina syndrome from other complications in which there is no acute pain.
Cauda equina syndrome is characterized by intense pain in the sacrum and lower back, which radiates to the buttocks, anogenital area and the back of the thigh. In some cases, paresis, peripheral paralysis and sensory disturbances occur. Severe cases are characterized by paralysis of the buttocks and both legs. A characteristic feature of complications can be considered asymmetry of sensory and motor disorders.
Lumbar osteochondrosis can cause the development of the myelogenous syndrome "intermittent claudication" in which weakness in the legs occurs when walking, frequent urge to urinate and numbness in the lower part of the torso. The cause of this problem is poor blood supply to the lower parts of the spinal cord. After rest, these feelings disappear.
Caudogenic "intermittent claudication" occurs with ischemia of the root of the cauda equina - goosebumps and tingling sensation when walking. Over time, this symptom can grow higher, reaching the perineum, genitals and groin. Weakness in the legs disappears after a short rest.
Compression of the Adamkiewicz artery can occur due to unsuccessful sudden movement, heavy lifting, or shaking. This complication of osteochondrosis of the lumbar spine is manifested by disorders of the pelvic organs, loss of sensitivity, the appearance of bedsores and leg muscle atrophy.
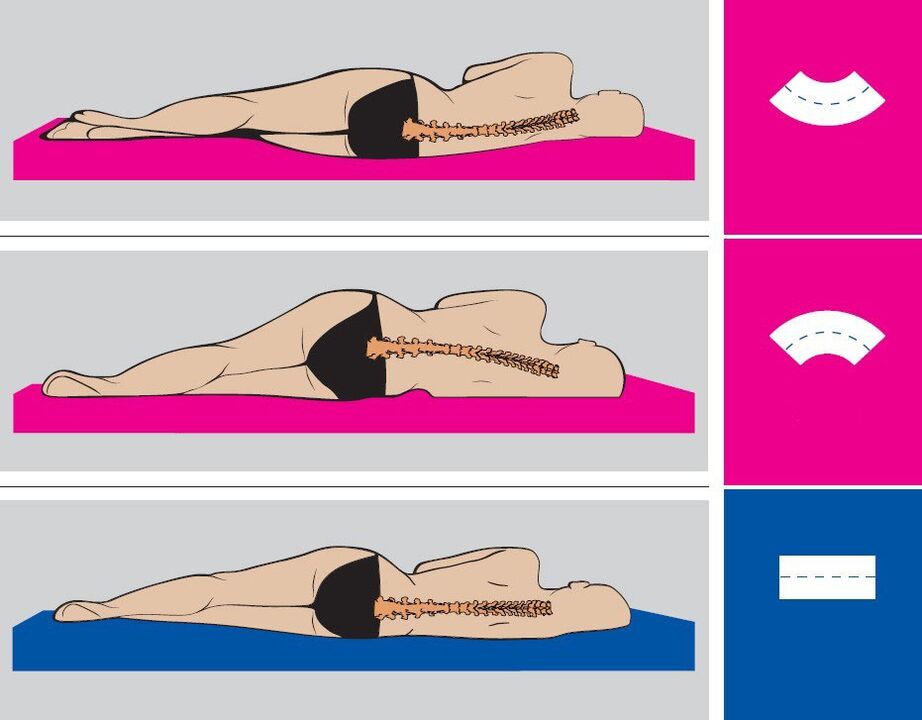
Osteochondrosis of the lumbar spine is manifested by painful pain in the lower back. Due to a longer stay in an uncomfortable position, the pain may increase. After sleeping or resting in a lying position, the pain decreases or disappears completely.
The appearance of stressful situations for the body can cause the development of an acute condition. Most often it happens during hypothermia, heavy loads and sudden movements. Exacerbation is characterized by severe pain, which can descend from the lumbar region to the legs. The body can independently try to reduce the load on the affected part of the spine by strongly tensing the muscles of the lower back. A patient with osteochondrosis of the lumbar spine tries to find a comfortable position in which the pain decreases.
Diagnosis of lumbar osteochondrosis
The diagnosis of osteochondrosis is carried out in several stages. The doctor should talk to the patient, inquire about the complaints, learn about the nature of the pain, where it is localized, at what time painful sensations are felt, their duration, intensity, etc. In addition, the doctor will find out under what conditions the pain appears, when it increases or decreases.
After that, the vertebrologist examines the medical history, i. e. medical history. The doctor will certainly clarify how long the painful condition lasts, what was the cause of the pain and how you feel in the period when the pain disappears. An important point is the preliminary treatment, as well as the effectiveness of certain treatment methods. A qualified doctor will certainly ask the patient about living and working conditions, range of motion, well-being under certain loads and past illnesses. It is very important to determine whether the patient had spinal injuries, whether he was involved in sports and whether any of his close relatives had spinal diseases.
The next step in the diagnosis is the examination of the patient. The doctor will pay attention to the position of the head, legs and arms in relation to the body, gait, posture, symmetry of the body parts, the condition of the skin on the damaged area and the patient's movements. After that, the range of motion of the spine and the degree of damage are determined. To do this, the doctor will ask the patient to bend forward, sideways, backward, ask him to move different parts of his back and tilt his head. A healthy person should not experience any creaking or joint pain during such a simple test.
If the patient does not suffer from osteochondrosis, then the chin can reach the chest and shoulders. Head movements in each direction are about 60 degrees. A 45-degree angle is created by bending to the side between the head and the upper part of the cervical spine. The distance from the sacrum to the spinous process of the seventh cervical vertebra increases by 5-7 centimeters when bending forward. This distance is reduced by 5-6 cm when bending backwards. An experienced vertebrologist will pay attention to how the knee and hip joints participate in bending and how the configuration of the spine changes.
Treatment of osteochondrosis of the lumbar spine
Lumbar osteochondrosis requires complex, intensive and long-term treatment. This is especially true for chronic cases with multiple intervertebral hernias and protrusions.
Effectivetreatment of osteochondrosis of the lumbar spineit is achieved by reflex methods that do not cause side effects, but bring maximum benefit. Remember, recovery from such a serious illness cannot come quickly. In every case of lumbar osteochondrosis, the doctor prescribes an individual treatment regimen.

It is worth noting that manual therapy can be used only in cases where the patient's spine is not damaged by protrusions and intervertebral hernias. The integrated use of these techniques allows you to restore normal blood microcirculation, eliminate congestion, vascular edema, relieve muscle spasms, restore the balance of metabolic processes in the tissues of the vertebrae and intervertebral discs, and also improve tissue nutrition in the lumbar region. As a result, the natural regeneration process is stimulated. It is important to note that in the case of lumbar osteochondrosis, manual therapy should be aimed at improving the functions of the spine.
Lumbar osteochondrosis treatment procedures are complemented by the use of herbal medicines that improve innervation in the body and also restore the balance of metabolic processes. The vertebrologist will recommend to patients the correction of diet and a more active lifestyle. It is important to adjust your body weight, because excess weight puts additional pressure on the lower back and also makes it difficult to develop osteochondrosis of the lumbar spine.
An experienced specialist who treats osteochondrosis allows the patient to achieve serious results, as well as avoid surgery, improve motor activity, eliminate pain in the lower back and comprehensively improve the body to prevent further deterioration. Acute pain disappears after 1-3 sessions of manual therapy, and a positive treatment effect is achieved on average after 10-15 sessions. Remember that the timely start of treatment is a guarantee of achieving positive results.
In the period of worsening lower back pain, the patient is recommended to stay in bed for 2-3 days. Nonsteroidal anti-inflammatory drugs, painkillers, venotonics, diuretics, nicotinic acid, B vitamins are prescribed for quick pain relief. Walking with crutches, dry or underwater traction of the spine can also be prescribed to relieve the spine. If necessary, glucocorticoid blocks or paravertebral blocks with anesthetic are prescribed.
Physiotherapy treatment of osteochondrosis of the lumbar spine may include electrophoresis, laser therapy and ultraviolet radiation. Physical therapy is a mandatory component of a comprehensive treatment program. Some exercises can be used in the acute phase, but almost all exercises are recommended after the pain has subsided. Regular physical exercises restore tissue nutrition, improve the supply of blood and lymph to the intervertebral discs, and gradually restore the flexibility and elasticity of the joints and cartilage. Thus, the patient's condition improves, and the interval between periods of deterioration increases.
Spa treatment also has a good effect on health. In climatic resorts, iodine-bromine, hydrogen sulphide and radon baths are prescribed.
Surgical methods of treatment are used only if the patient's pain cannot be alleviated by conservative methods for a long time, with paresis of the muscles of the lower extremities and disruption of the process of natural urination and defecation. During the operation, the herniated disc is removed and the spinal segment is strengthened.
Prevention of lumbar osteochondrosis
Prevention of lumbar osteochondrosis consists in following simple rules recommended by a vertebrologist. Remember that the development of the disease can be prevented only by carefully following these rules, no matter what:
- Keep your lower back dry and warm, don't chill your spine and avoid drafts.
- Do not lift heavy objects or carry them over long distances.
- Try not to make sudden movements.
- Maintain proper posture during work and rest.
- Change your position as often as possible, trying not to stay in one position for too long.
- Do physical therapy.
- Try not to stay in a bent position for too long.
- When cleaning, use long cloths, a broom and a vacuum cleaner with a long hose so you don't have to bend over.
- Lift weights correctly: bend over with a straight back or bend your knees, lift the bags with a straight back and stand up straight. Keep your arms with the load as close to your body as possible.
- If you need to bend low to pick something up off the floor, such as under a table or bed, get down on one knee and keep your back straight.
- Distribute the weight equally between the two hands.
- Strengthen the gluteal muscles, stretch the spine, walk every day.
- Balance your diet, enrich your diet with dairy and plant products.
- Adhere to the drinking regimen - 1. 5-2 liters of water and herbal teas per day.
- Get rid of bad habits - alcohol, smoking, drugs.



















